Preventing Serious Brain Damage From Nerve Agents
New UC Davis CounterACT Center to Improve Medical Response
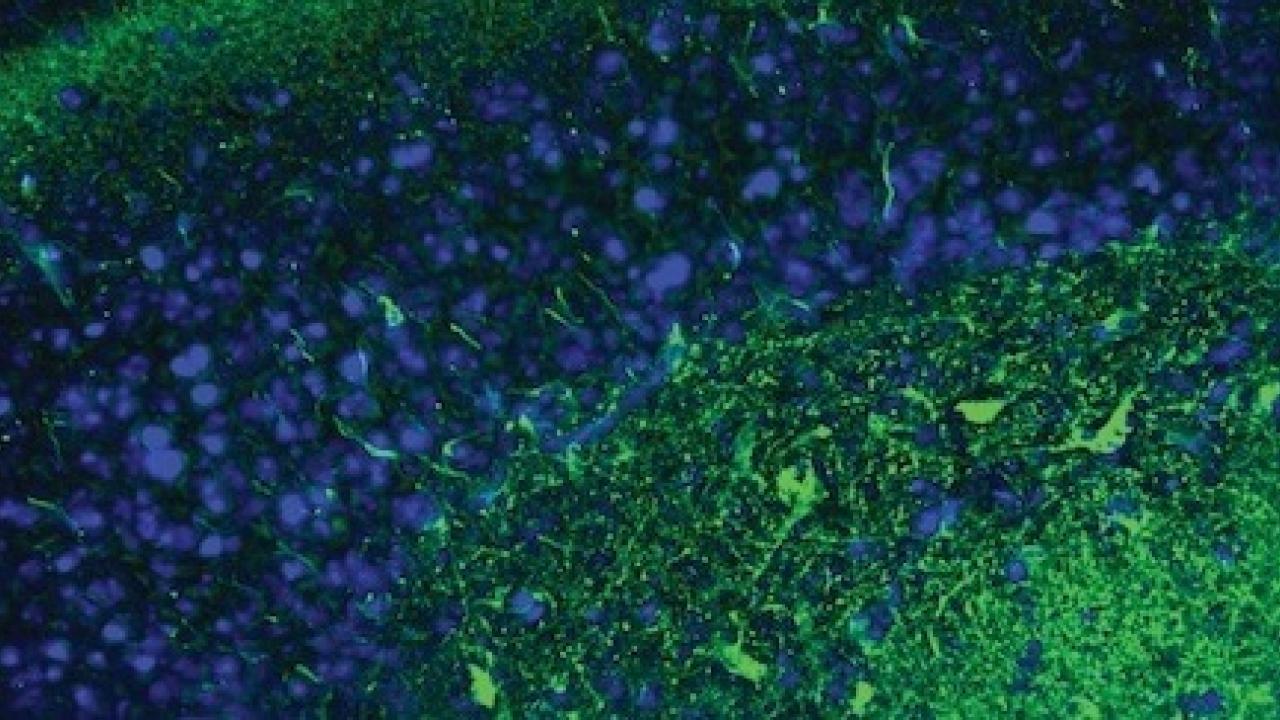
The University of California, Davis, is establishing a new center designed to develop ways to prevent long-term brain damage in humans when poisoned by organophosphate chemical nerve agents or pesticides. These organophosphates are a group of human-made chemicals developed for warfare during World War II and then subsequently modified for use as pesticides. They can affect insects and mammals, causing recurrent seizures and nervous system damage.
The National Institute of Neurological Disorders and Strokes has awarded a five-year, $13.7 million grant for a new UC Davis CounterACT Center of Excellence. The center will focus on new treatments and strategies to prevent long-term consequences after chemical nerve agent exposure.
Currently, doctors and first responders can give people several drugs to either prevent or acutely treat seizures following poisoning with organophosphates, said UC Davis School of Veterinary Medicine toxicologist Pamela Lein, who will serve as the center’s director.
“However, these drugs must be given quickly, often within 20-30 minutes of exposure, and that is usually not the case in a mass casualty event, terrorist attack or an industrial accident,” Lein said. “The goal of the CounterACT Center of Excellence is to develop therapeutic strategies to prevent significant nervous system damage if this standard of care is delayed.”
Long-term effects from exposure
Without immediate treatment, people can have substantial long-term injury from these chemicals, said Amy Brooks-Kayal, professor and chair of the neurology department at the UC Davis School of Medicine. She will serve as the center’s co-director.
“Survivors often have problems with memory, thinking and cognition,” said Brooks-Kayal. “They often will go on to have epilepsy, which is spontaneous recurrent seizures, after these events. What’s unique about this new CounterACT center is that we’re focusing on how we can make sure those who do survive are able to live their best lives.”
Researchers are hoping the treatments they develop will also help people who may develop seizures after traumatic brain injuries, stroke or prolonged seizures secondary to fever, illness or other causes. Results could also help both people and companion animals, particularly dogs and horses, who have drug-resistant seizures.
“I hope a chemical attack will never happen, but this research has implications for things that happen all the time, such as accidental pesticide exposures or acquired epilepsy,” Brooks-Kayal said. “We might be able to make lives better for people developing epilepsy in the future. That to me is very exciting.”
The interdisciplinary center will be housed in the UC Davis School of Veterinary Medicine. Researchers include Pam Lein and Fred Gorin with the School of Veterinary Medicine; Amy Brooks-Kayal, Angie Gelli, Marco González, Gene Gurkoff, Jill Silverman, Heike Wulff, Daniel Tancredi and Danielle Harvey with the School of Medicine; Bruce Hammock and Jun Yang with the College of Agricultural and Environmental Sciences; and Abhijit Chaudhari and Brad Hobson with the College of Engineering.
Media Resources
Media Contacts:
- Pamela Lein, School of Veterinary Medicine, pjlein@ucdavis.edu
- Amy Brooks-Kayal, School of Medicine, abkayal@ucdavis.edu
- Amy Quinton, News and Media Relations, 530-601-8077, amquinton@ucdavis.edu
